Medical Billing vs. Medical Coding: What’s the Real Difference?
Medical billing is the process of submitting and following up on insurance claims to ensure healthcare providers get paid for their services. Medical coding, on the other hand, involves translating diagnoses, treatments, and procedures into standardized codes used for documentation and billing. In short: coders assign the codes, and billers use those codes to generate claims and collect payment.
Medical billing and medical coding are critical components of the modern healthcare system. Although often grouped together or used interchangeably, they are distinct professions with unique roles, responsibilities, and impacts. Understanding the real difference between medical billing and medical coding is essential—not only for those considering a career in healthcare administration but also for medical providers, insurers, and patients who rely on accurate, efficient processes to ensure timely reimbursement and clear communication.
This in-depth guide will explore what medical billing and medical coding entail, how they work together, what skills each role requires, and why the distinction matters. Whether you’re a healthcare professional, student, or simply curious, this article will help you grasp the core differences and synergies between the two.
Read more: 5 Ways Medical Billing Outsourcing Can Improve Your Hospital
What Is Medical Coding?
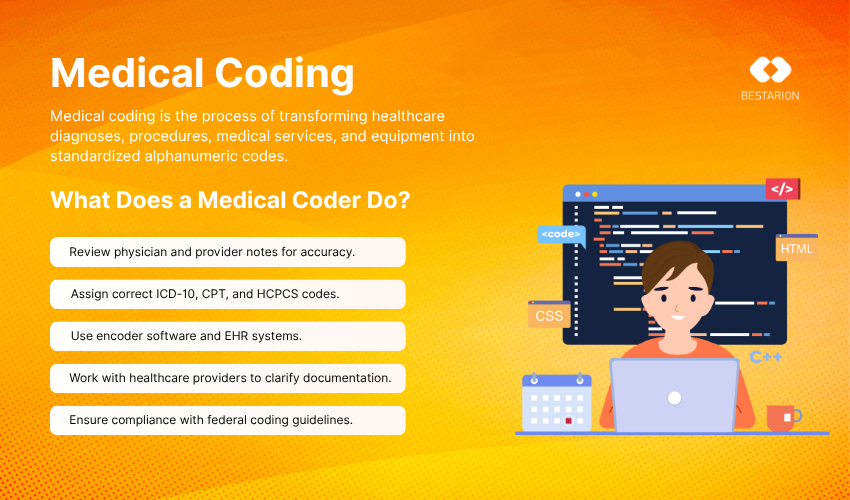
Medical coding is the process of translating healthcare diagnoses, procedures, medical services, and equipment into universal alphanumeric codes. These codes are drawn from a few standardized code sets:
-
ICD-10-CM (International Classification of Diseases, 10th Revision, Clinical Modification) for diagnoses.
-
CPT® (Current Procedural Terminology) for medical procedures.
-
HCPCS Level II (Healthcare Common Procedure Coding System) for equipment, supplies, and some services not included in CPT.
Purpose of Medical Coding
The primary goal of medical coding is to ensure that every service provided by a healthcare professional is accurately documented using universally recognized codes. These codes serve several purposes:
-
Standardization: Allowing different healthcare and insurance systems to communicate consistently.
-
Billing Accuracy: Ensuring the right services are billed and reimbursed.
-
Data Collection and Research: Enabling analysis of healthcare trends, treatments, and outcomes.
What Does a Medical Coder Do?
A medical coder reviews patient records, including physician notes, lab results, and procedure reports. They extract the relevant information and assign the appropriate codes using specialized software and coding manuals. Accuracy is critical because incorrect codes can lead to claim denials, revenue loss, and compliance issues.
Required Skills for Medical Coders
-
Deep knowledge of anatomy, physiology, and medical terminology.
-
Proficiency with coding systems and healthcare documentation.
-
Analytical and detail-oriented mindset.
-
Familiarity with regulatory guidelines like HIPAA and payer policies.
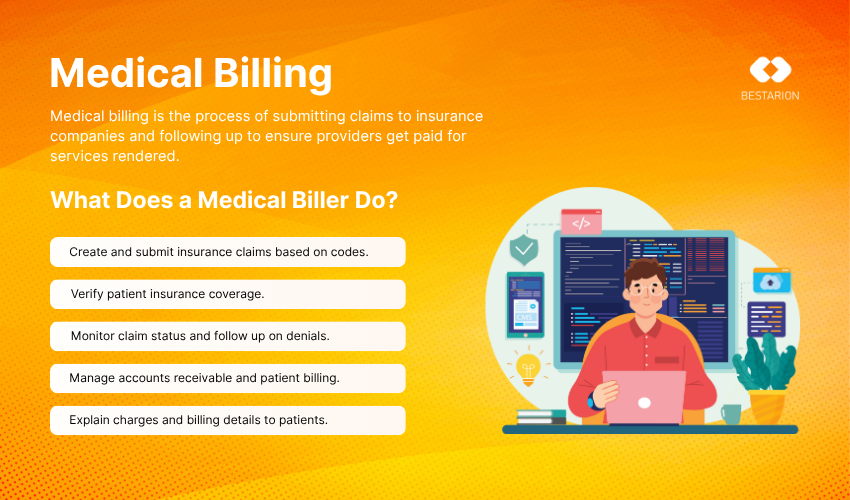
What Is Medical Billing?
Medical billing is the process of submitting, following up on, and appealing claims with health insurance companies to receive payment for services rendered by a healthcare provider. While medical coding lays the groundwork, medical billing brings the financial process to completion.
Purpose of Medical Billing
Medical billing ensures that providers are paid for their services in a timely and accurate manner. Billers are responsible for preparing invoices and communicating with insurance companies and patients to resolve payment issues.
What Does a Medical Biller Do?
A medical biller uses the codes generated by medical coders to create insurance claims and patient invoices. Their role includes:
-
Verifying patient insurance coverage and eligibility.
-
Creating and submitting claims to payers (insurance companies, Medicare, Medicaid).
-
Following up on unpaid or denied claims.
-
Sending patient bills for outstanding balances.
-
Working with insurance companies to resolve billing issues.
Required Skills for Medical Billers
-
Strong knowledge of insurance guidelines and reimbursement processes.
-
Understanding of coding and medical terminology.
-
Customer service and communication skills.
-
Familiarity with medical billing software like Kareo, AdvancedMD, or Athenahealth.
Key Differences Between Medical Billing and Medical Coding
Medical coding involves translating healthcare services into standardized codes (like ICD-10 or CPT), while medical billing uses those codes to create and submit claims to insurance companies for payment. Coders focus on documentation accuracy; billers handle claim submission, payment tracking, and resolving rejections.
Both functions are essential to ensure healthcare providers get paid accurately and efficiently, but they operate at different stages of the revenue cycle and require different skills.
Here’s a detailed comparison to highlight their unique roles, tools, and responsibilities:
| Aspect | Medical Coding | Medical Billing |
|---|---|---|
| Core Function | Converts healthcare services into universal alphanumeric codes | Uses those codes to create and submit insurance claims for reimbursement |
| Process Role | Happens first—sets the foundation for billing | Follows coding—initiates claim submission and follow-up |
| Key Tools Used | ICD-10-CM, CPT®, HCPCS manuals, EHR documentation | Billing software (Kareo, AdvancedMD, Athenahealth), clearinghouses |
| Main Focus Area | Accuracy in clinical documentation and coding compliance | Maximizing reimbursement while minimizing claim rejections |
| Communication | Limited direct contact; mostly back-office work with medical documentation | Regular interaction with insurance companies, patients, and sometimes providers |
| Specialized Knowledge | Deep understanding of medical terminology, procedures, and coding guidelines | In-depth knowledge of insurance plans, payer rules, and patient billing regulations |
| Certifications | CPC, CCS, CCA (from AAPC or AHIMA) | CPB, CMRS, or on-the-job training combined with software experience |
| Career Environment | Hospitals, physician offices, third-party coding firms, remote work | Hospitals, billing companies, private practices, remote or hybrid roles |
Why This Difference Matters to You
If you’re exploring a career in healthcare administration
Understanding whether you are more detail-oriented and analytical (coding), or people-focused and strategic (billing), can help you pick the career that matches your strengths. Medical coders work more behind-the-scenes, diving deep into clinical records and assigning the correct codes. Medical billers work closer to the revenue end, ensuring that claims are processed correctly and payments are received.
If you’re a healthcare provider or clinic manager
Recognizing the distinction between these two roles helps you hire smarter and optimize your internal processes. Hiring a certified coder improves coding accuracy and compliance, reducing denials. A knowledgeable medical biller ensures timely reimbursement and fewer payment delays. Together, they improve cash flow and reduce administrative overhead.
If you’re a patient navigating medical bills and insurance
Knowing who to talk to can save time and frustration. For questions about what your procedure was coded as or potential errors, reach out to a medical coder or medical records department. For questions about your bill, coverage, or payment plans, a medical billing department is your best resource.
How Medical Billing and Coding Work Together
Although separate roles, medical billing and coding are interconnected. The coding process directly impacts the accuracy and success of medical billing. Here’s how they typically function in sequence:
-
Patient Visit: A patient visits a healthcare provider for a consultation, treatment, or procedure.
-
Documentation: The healthcare provider documents the visit, detailing symptoms, diagnoses, and treatments.
-
Medical Coding: The coder reviews the documentation and assigns the correct codes.
-
Claim Preparation: The biller uses these codes to prepare an insurance claim.
-
Claim Submission: The claim is sent to the insurance company for payment processing.
-
Reimbursement or Follow-Up: The insurance company reimburses the provider or returns the claim for correction or clarification.
Without proper coding, billing cannot be executed accurately. Similarly, without effective billing, proper codes won’t translate into timely payments.
Read more: Ensuring HIPAA Compliance in Medical Billing: A Comprehensive Handbook
Training and Certification: How to Become a Medical Biller or Coder
Medical Coding Certification
Most employers require certification from a reputable organization. Common options include:
-
AAPC Certified Professional Coder (CPC)
-
AHIMA Certified Coding Associate (CCA) or Certified Coding Specialist (CCS)
Training typically involves courses in anatomy, physiology, medical terminology, and hands-on coding practice.
Medical Billing Certification
While not always required, certification can significantly boost job prospects:
-
Certified Professional Biller (CPB) by AAPC
-
Certified Medical Reimbursement Specialist (CMRS)
Training includes instruction in insurance procedures, payer requirements, patient billing, and compliance.
Medical Billing or Coding: Which Path Is Right for You?
If you’re considering entering the healthcare industry without spending years in school, both medical billing and coding offer strong job security, competitive salaries, and remote work opportunities. But they suit different personality types and strengths:
-
Choose Medical Coding if you enjoy problem-solving, analyzing detailed information, and working independently with clinical data.
-
Choose Medical Billing if you enjoy communication, resolving issues, and working with numbers and insurance processes.
Still unsure? Many professionals start in one role and cross-train in the other, giving them flexibility and making them more competitive in the job market.
Career Outlook and Salary Comparison
According to the U.S. Bureau of Labor Statistics (BLS), both fields are projected to experience steady growth due to increasing healthcare demands and regulatory complexity.
-
Medical Coders typically earn between $45,000 and $70,000 annually, depending on experience and certification.
-
Medical Billers may earn $40,000 to $65,000 annually, with top earners in hospital settings or specialized practices.
Those who are cross-trained in both billing and coding may find more opportunities and higher salaries.
Challenges and Opportunities in Medical Billing and Coding
Common Challenges
-
Frequent Coding Updates: Keeping up with changing ICD, CPT, and HCPCS codes.
-
Insurance Payer Complexity: Navigating multiple payers with unique requirements.
-
Claim Denials: Identifying and resolving reasons for claim rejections.
-
Compliance and Regulations: Staying compliant with HIPAA and medical necessity rules.
Opportunities for Growth
-
Remote Work Flexibility: Many positions offer telehealth-compatible roles.
-
Specialization Options: Oncology, radiology, cardiology coding, or billing for specific payer types.
-
Career Advancement: With experience, professionals can move into auditing, compliance, or supervisory roles.
Why the Difference Matters for Providers and Patients
For Healthcare Providers
Understanding the distinction ensures the right personnel are in place for efficient revenue cycle management. It helps providers:
-
Reduce billing errors and claim denials.
-
Shorten the payment cycle.
-
Improve documentation and compliance.
For Patients
Clear medical coding and accurate billing contribute to transparent communication and fewer billing surprises. It can prevent:
-
Overcharges due to incorrect codes.
-
Insurance denials based on mismatched data.
-
Frustrating back-and-forth on disputed claims.
Frequently Asked Questions (FAQs)
1. Can one person do both medical billing and coding?
Yes. In smaller practices, a single professional may handle both roles. However, due to the complexity and workload, larger organizations typically separate the two.
2. Which is harder, medical billing or medical coding?
Medical coding requires a deeper understanding of anatomy, procedures, and code sets. Medical billing involves more communication, insurance knowledge, and troubleshooting skills. Each role has its unique challenges.
3. Do I need a degree to become a medical coder or biller?
A degree is not mandatory. Most employers accept certifications from organizations like AAPC or AHIMA, often earned after completing a postsecondary training program.
4. How long does it take to become a certified coder or biller?
Training programs typically last between 4 to 12 months, depending on the depth and whether the program is part-time or full-time.
5. Is there a demand for medical billing and coding professionals?
Yes. As the healthcare industry grows and documentation requirements increase, the need for skilled billers and coders continues to rise.
Final Thoughts
Medical billing and medical coding may work hand-in-hand, but they are fundamentally different processes that require unique skills, training, and responsibilities. Coders focus on transforming healthcare services into accurate, standardized codes, while billers ensure those services are reimbursed properly by navigating the complex insurance landscape.
Understanding the real difference between these roles can help organizations staff effectively, streamline operations, and optimize financial performance. It can also guide aspiring professionals in choosing the right career path based on their strengths and interests.
As healthcare continues to digitize and expand, professionals who are skilled in either—or both—of these disciplines will play an increasingly critical role in maintaining operational efficiency and financial viability across the healthcare ecosystem.